#13,081
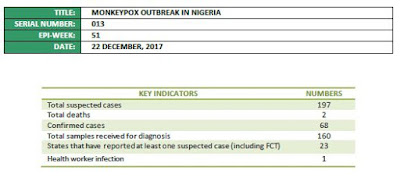
Beginning in September of 2017 - after an absence of nearly 40 years - Nigeria began to report scattered cases of suspected human Monkeypox (see map above). By December 22nd - the date of the last Nigerian CDC Update - the number of suspected cases across 23 states was nearing 200 (see chart below).
The name `monkeypox’ is a bit of a misnomer. It was first detected (in 1958) in laboratory monkeys, but further research has revealed its host to be rodents or possibly squirrels. It produces a remarkably `smallpox looking' illness in humans, albeit not as deadly.
Humans can contract it in the wild from an animal bite or direct contact with the infected animal’s blood, body fluids, or lesions, but consumption of under cooked bushmeat is also suspected as an infection risk. Human-to-human transmission is also possible.
According to the CDC: There are two distinct genetic groups (clades) of monkeypox virus—Central African and West African. West African monkeypox is associated with milder disease, fewer deaths, and limited human-to-human transmission.Monkeypox is most commonly found in the Central Africa countries of the DRC and the CAR - where outbreaks have been on the rise for years (see here and here) - presumably because smallpox vaccinations (which provided up to 85% protection) were halted in the late 1970s.
While Nigeria's Monkeypox outbreak appears to be waning, the obvious question remains : how did the virus reappear nearly 40 years after the last recorded outbreak in Nigeria?The two most likely possibilities are an imported case from the DRC or the CAR, where outbreaks remain common, or a recent zoonotic spillover from local reservoir hosts.
To try to answer that question, 29 isolates were sent to an outside lab which sequenced them in order to determine their origins.As an excerpt from the following Lancet correspondence explains, this appears to be the result of a local zoonotic spillover. First a link to the report, after which I'll return with a postscript.
Genomic characterisation of human monkeypox virus in Nigeria
Ousmane Faye, Catherine B Pratt, Martin Faye, Gamou Fall, Joseph A Chitty, Moussa M Diagne, Michael R Wiley, Adesola F Yinka-Ogunleye, Sola Aruna, Ebitimitula N Etebu, Neni Aworabhi, Dimie Ogoina, Wari Numbere, Nwando Mba, Gustavo PalaciosEmail the author Gustavo Palacios, Amadou A Sall, Chikwe Ihekweazu
Published: 16 January 2018
PlumX Metrics
DOI: http://dx.doi.org/10.1016/S1473-3099(18)30043-4
(EXCERPT)
Phylogenetic analysis (appendix) indicates that the closet relative of the three outbreak isolates were the two Nigerian strains available on GenBank (KJ642615 and KJ642617), within the west African clade. The isolates grouped most closely to KJ642617, a genome isolated from a human MPXV case in Ihie, Abia State, Nigeria, in 1971, which is relatively close to the epicentre of the current outbreak.
These findings support the hypothesis that the index case of the current outbreak in Nigeria was not imported, but probably originated from a spillover event or events involving reservoir hosts. These results emphasise the value of local surveillance for the early detection of viral spillovers and the need for advanced characterisation to help determine the origins of outbreaks.
(Continue . . . )
As the percentage of smallpox vaccinated members of the community dwindles, the risks of human MPXV outbreaks is only expected to increase (see 2010 PNAS study Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo).
A 2016 study (see EID Journal:Extended H-2-H Transmission during a Monkeypox Outbreak) looked at a large 2013 outbreak of Monkeypox in the DRC and suggested that the virus's epidemiological characteristics may be changing (possibly due to the waning smallpox vaccine derived immunity in the community).
The DRC had reported a 600% increase in cases over both 2011, and 2012. The authors also cite a higher attack rate, longer chains of infection, and more pronounced community spread than have earlier reports.Like all viruses, Monkeypox continues to evolve and diversify, as discussed in the 2014 EID Journal article Genomic Variability of Monkeypox Virus among Humans, Democratic Republic of the Congo, where the authors cautioned:
Small genetic changes could favor adaptation to a human host, and this potential is greatest for pathogens with moderate transmission rates (such as MPXV) (40). The ability to spread rapidly and efficiently from human to human could enhance spread by travelers to new regions.Although Monkeypox is normally restricted to small outbreaks in Africa, in 2003 we saw a rare outbreak in the United States when a Texas animal distributor imported hundreds of small animals from Ghana, which in turn infected prairie dogs that were subsequently sold to the public (see MMWR Update On Monkeypox 2003).
By the time this outbreak was quashed, the U.S. saw 37 confirmed, 12 probable, and 22 suspected human cases. Among the confirmed cases 5 were categorized as being severely ill, while 9 were hospitalized for > 48 hrs; although no patients died (cite).A reminder, as if we needed one, that in this highly mobile 21st century that outbreaks of rare and exotic diseases - even those occurring the most remote areas of the world - can be exported to anywhere on the globe in a matter of hours or days.
And so we watch outbreaks, such as this one in Nigeria, with considerable interest.