#18,013
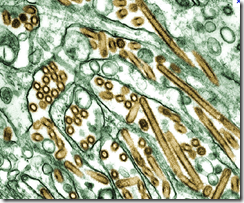
Yesterday researchers from the Department of Veterinary Diagnostic and Production Animal Medicine, College of Veterinary Medicine, at Iowa State University published a preprint with additional detailed information the HPAI H5N1 virus that spilled over from birds into cows - and a human and several cats - in Texas earlier this year (see graphic above).
While the exact route of introduction of the virus to cattle remains unknown, based on the available evidence, the authors hypothesize:
. . . wild birds may spread the virus through direct contact or contamination of water sources or feed staffs utilized by dairy cattle or other animals such as skunks. Consequently, other cattle in the herd, workers and domestic felids on dairy farms may contract the virus through direct contact with infected cattle or after consuming raw colostrum and milk from infected cattle. The detection of the same strain of HPAI viruses in various wild bird species, such as blackbirds and common grackles in Texas and Canada geese in Wyoming (Central Flyway), provides further support for this hypothesis.
Another potential transmission scenario involves bovine-to-bovine spread. Recently, the USDA has verified the presence of this HPAI virus strain in dairy herds located in Idaho, Michigan, Ohio, North Carolina, and South Dakota (Link). In these cases, a documented history exists of cattle introduction from farms in the initial outbreak area, further supporting the hypothesis that lateral transmission can occur among cattle.
Although human infections with this relatively new HPAI H5N1 clade 2.3.4.4b virus remain rare, the authors write:
. . . 37 new mammal species have been afflicted since 2021. The majority of these cases involve wild terrestrial mammals such as foxes, skunks, bears, bobcats, and raccoons (9, 23, 24). Intriguingly, there have been sporadic infections among domestic pets like domestic cats and dogs (25), as well as marine mammals, including dolphins and sea lions (26).
Moreover, from January 2022 to April 2023, eight documented human cases of H5N1 influenza from clade 2.3.4.4b have been recorded, several of which were severe or fatal (https://www.cdc.gov.flu/), underlining the gravity of this situation.
I've reproduced the link, and some excerpts from this 19-page public domain summary below, but you'll want to follow the link to read it in its entirety.
Highly Pathogenic Avian Influenza A (H5N1) clade 2.3.4.4b Virus detected in dairy cattle
Xiao Hu, Anugrah Saxena, Drew R. Magstadt, Phillip C. Gauger, Eric Burrough, Jianqiang Zhang, Chris Siepker, Marta Mainenti, Patrick Gorden, Paul Plummer, Ganwu Li
doi: https://doi.org/10.1101/2024.04.16.588916
This article is a preprint and has not been certified by peer review
Preview PDF
Abstract
The global emergence of highly pathogenic avian influenza (HPAI) A (H5N1) clade 2.3.4.4b viruses poses a significant global public health threat. Until March 2024, no outbreaks of this virus clade had occurred in domestic cattle. We genetically characterize HPAI viruses from dairy cattle showing an abrupt drop in milk production. They share nearly identical genome sequences, forming a new genotype B3.13 within the 2.3.4.4b clade.
B3.13 viruses underwent two reassortment events since 2023 and exhibit critical mutations in HA, M1, and NS genes but lack critical mutations in PB2 and PB1 genes, which enhance virulence or adaptation to mammals. The PB2 E627K mutation in a human case underscores the potential for rapid evolution post-infection, highlighting the need for continued surveillance to monitor public health threats.
(SNIP)
In addition to being the first documented occurrence of HPAI A (H5N1) clade 2.3.4.4b virus infection in domestic dairy cattle, early pathology observations in this outbreak revealed an apparent tissue tropism for mammary gland in lactating domestic dairy cattle (personnel communication).
Prior to this incident, the clade 2.3.4.4b IAV has typically caused systemic and respiratory diseases in wild mammals (9). Gross and microscopic lesions in wild mammals were frequently observed in organs such as the lung, heart, liver, spleen, and kidney, with some cases resulting in lesions in the brain leading to neurological signs.
Furthermore, while it is widely recognized that certain strains of HPAI H5N1 clade 2.3.4.4b virus can breach the blood-brain barrier (9, 23, 25, 27), this is the first instance where the virus may penetrate the blood-milk barrier and be present in milk, raising potential public health concerns.
(SNIP)
Notably, all HPAI viruses originating from dairy cattle and cats exhibit consistent amino acid residues in the HA gene, including 137A, 158N, and 160A, which have been documented to enhance the affinity of avian influenza viruses for human-type receptors (15, 16). Additionally, these dairy cattle derived and cat-derived HPAI viruses harbor key virulence-increasing amino acid residues, such as 30D, 43M, and 215A in M1 (17-19), as well as 42S, 103F, and 106M in NS1(20).
The presence of these amino acid mutations raises legitimate concerns regarding the potential for cross-species transmission to humans and other mammalian species. It is noteworthy that crucial mutations associated with mammalian host adaptation and enhanced transmission, specifically residues 591K, 627K/V/A, 701N, in PB2 (18, 21, 22), and 228S, along with the virulence increasing residue 66S in PB1-F2(30), were conspicuously absent in all HPAI virus strains derived from dairy cattle and cats.
This observation suggests that the current overall risk to human health is relatively low. However, it is imperative to recognize that influenza viruses have the capacity for rapid evolution within their host environments post-infection. A recent human case with direct contact with infected dairy cattle revealed a genetic change (PB2 E627K) (LINK), indicating the potential for adaptation or transmission events. This underscores the dynamic nature of influenza viruses and the importance of continued surveillance and vigilance in monitoring potential threats to human health.
Over the past two years nearly half the states in the country haven't reported a single spillover - and while infected animals may die in remote and difficult to access places where their carcasses are quickly scavenged - this probably speaks more to our reluctance to aggressively look for cases than how often they actually occur.
While the USDA cites logistical problems and concerns over laboratory capacity, we appear embarked on a similar path with livestock testing, which remains both limited and voluntary.
As long as the virus remains poorly adapted to humans, it is possible what we don't know won't hurt us. But given the enormous strides HPAI H5 has made over the past 3 years, any purported `bliss from ignorance' may prove short-lived.